Infertility workup testing involves a comprehensive evaluation to identify potential factors contributing to difficulties in conceiving. This process typically includes various examinations and procedures aimed at assessing both partners' reproductive health.
Blood tests may be performed to evaluate hormone levels, including follicle-stimulating hormone (FSH), luteinizing hormone (LH), AMH, Prolactin, thyroid function, and others, to assess ovarian function and overall reproductive health.
For men, a semen analysis is essential to assess sperm count, motility, morphology, and other parameters that affect sperm quality and fertility.
Women may undergo ovulation monitoring through blood tests and/or ultrasound examinations to track hormone levels and follicle development throughout the menstrual cycle.
This imaging procedure involves injecting a contrast dye into the uterus and fallopian tubes to detect any blockages or abnormalities that may hinder conception.
An ultrasound examination may be performed to visualize the pelvic organs and detect any structural abnormalities in the uterus or ovaries.
In some cases, a minimally invasive surgical procedure called laparoscopy may be recommended to evaluate the pelvic organs directly, particularly in cases of suspected endometriosis or pelvic adhesions.
Typically, it is advised to test semen following an abstention period ranging from a minimum of 2 days to a maximum of 7 days. The professional responsible for conducting this examination is known as an Andrologist. Adhering to the WHO criteria for semen analysis is strongly advised by experts in the field. The Andrologist will evaluate your semen to assess various parameters, including:
Normal semen volume of a single ejaculate should be at least 1.5 ml.
Sperm count means the number of sperms present in your semen. 1 ml of semen should contain at least 15 million sperms. A concentration less than that is called Oligozoospermia.
A normal semen sample appears opalescent grey. Any deviation from this to red or yel-low may indicate presence of blood, infection etc.
Normal pH for semen is around 7.2. A higher or lower pH indicates infection or contam-ination respectively.
Morphology refers to the physical structure or form of something, such as the shape, size, and appearance of objects or organisms.
Motility refers to the ability of cells or organisms to move spontaneously and actively. In the context of sperm, it describes the ability of sperm cells to swim effectively, which is crucial for fertilization.

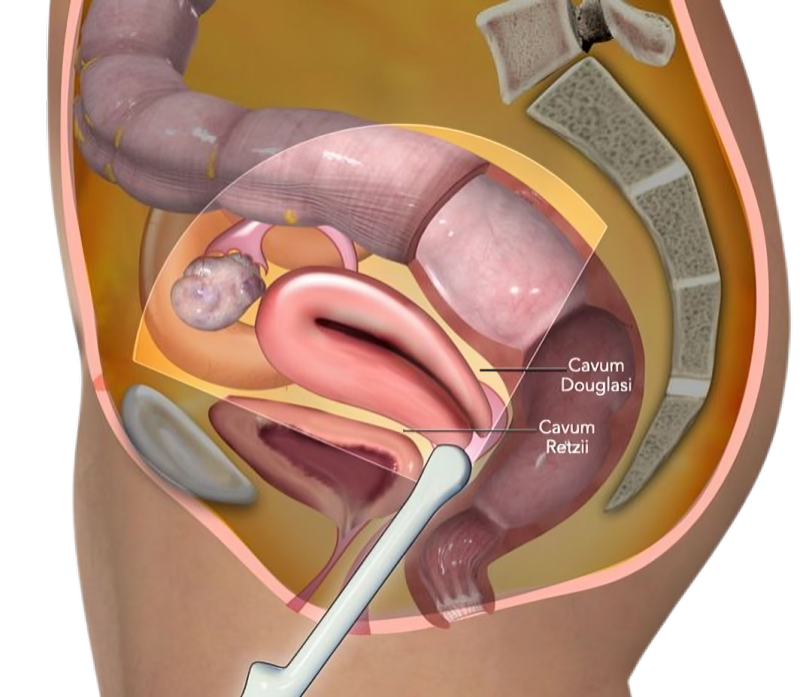
The process of a transvaginal ultrasound is typically not painful. It is somewhat more invasive compared to the standard ultrasound. Women may feel slight discomfort during the insertion of the transducer, but this usually diminishes shortly afterward.
A TVS might be advised for exploring unexplained pelvic discomfort, irregular menstrual cycles, inexplicable vaginal bleeding, or to evaluate fertility. Moreover, it is frequently employed in early pregnancy to verify the pregnancy, ascertain the gestational age, or screen for ectopic pregnancy.
Throughout pregnancy, the transvaginal ultrasound procedure is completely safe. The insertion of the transducer into the vagina does not pose any risk to the fetus's health. Additionally, a crucial point to note about transvaginal ultrasounds is that they do not involve radiation, further enhancing their safety during pregnancy.
A TVS typically lasts for approximately 15 to 30 minutes.
While a TVS may induce some discomfort, it should not be painful. Should you encounter pain during the scan, it's crucial to inform your doctor promptly.
While a TVS is generally deemed safe, there is always a slight risk of infection or bleeding linked with internal examinations. If you observe any unusual symptoms following the scan, such as pain, fever, or abnormal discharge, it is imperative to promptly contact your doctor.